What Does an Inverted T Wave on an ECG Indicate

T-wave inversion is a finding on an electrocardiogram (ECG) that reflects changes in the heart's electrical recovery phase or repolarization. While it can be a normal variant in some individuals, it also signals underlying cardiac conditions.
Inverted T waves are caused by a variety of causes, ranging from benign to life-threatening, including myocardial ischemia, previous heart attacks, pericarditis, electrolyte imbalances, and central nervous system disorders.
Pathological causes of T-wave inversions should be ruled out for timely diagnosis and treatment. T-wave inversion should never be evaluated in isolation; instead, patient symptoms, medical history, and other ECG findings should also be considered. T-wave inversion is important, and it helps us assess cardiac health.
T Wave on ECG
T-wave represents the ventricular repolarization of cardiac muscle cells after contraction. It follows the QRS complex and precedes the next P wave. The T-wave signifies electrical stability and overall heart health.
Ventricular repolarization and depolarization
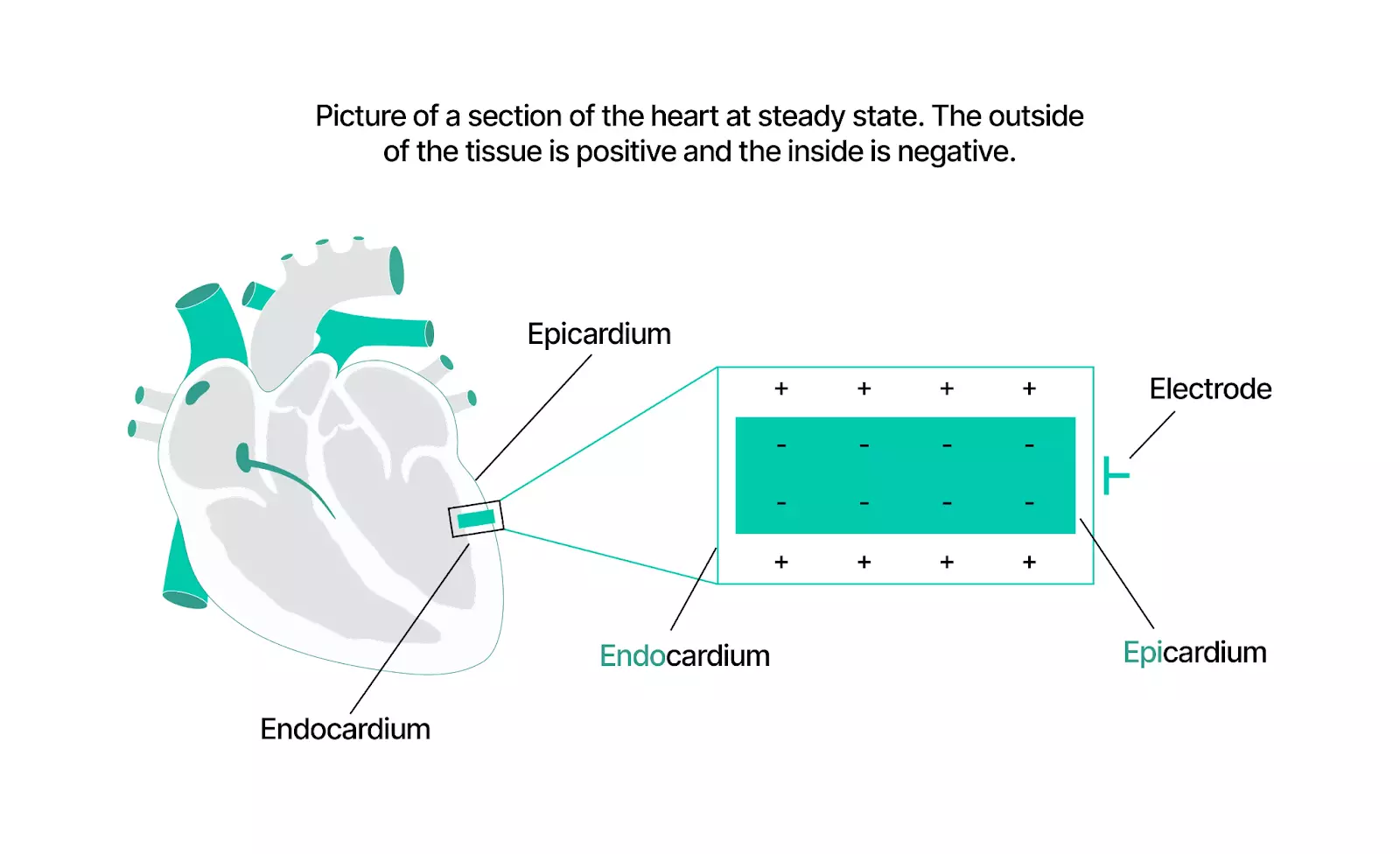
The heart's electrical activity controls how it pumps blood. The process involves two key phases.
Depolarization (contraction phase). When the heart contracts, positive ions enter the heart cells, making the inside of the cells positive and giving a signal to the ventricles to contract and pump blood. On the ECG, this is the QRS complex, the sharp spike.
Repolarization (relaxation phase). After a contraction, the heart needs to rest. Positive ions move out, giving the inside of the cells a negative charge. It allows the ventricles to relax and fill with blood for the next beat. On an ECG, this is seen as a T wave, a small upward wave after the QRS complex.
How does ECG see this process?
- When depolarization moves towards the ECG electrode, it shows an upward spike(positive)
- After a slight pause (ST segment a flat line), repolarization occurs in the same direction, forming an upright T wave.
Simply QRS = heart contraction.
T wave = heart relaxation.
The ECG captures these electrical changes, helping doctors assess the heart function.
Normal T wave characteristics
The normal T wave has been described as a gradual upstroke with a more rapid downstroke in the terminal portion. This relative asymmetry may vary because many females and elderly individuals, without identifiable cardiac disease, may have symmetric T waves.
- The T wave is normally upright in leads I, II, and V2 to V6
- Inverted in lead aVR and variable in leads III, aVL, aVF, and V1
- An inverted T wave in a single lead in one anatomic segment is unlikely to represent acute pathology; for instance, a single inverted T wave in either lead III or aVF can be a normal variant
Understanding T wave inversion
T-wave inversions on ECG can mean different things, but they generally fall into two categories.
Primary T wave inversion. These happen due to changes in heart electrical activity without any disruption in how the heart beats. They can be harmless, as in young people, or serious, as seen in heart attacks and brain injuries.
Secondary T wave inversion occurs when the heart's normal rhythm is restricted, often due to conditions like bundle branch blocks, abnormal electrical signals, pacemakers, or certain heart rhythm disorders.
Causes of T wave inversions
- Heart-related causes a heart attack. Past or ongoing blocked arteries or heart muscle thickening can lead to T-wave inversions.
- Lung-related causes a pulmonary embolism. Blood clots in the lungs can cause T-wave abnormalities.
- Brain-related causes: Strokes, brain bleeds, or seizures can sometimes show up as deep T wave inversions on an ECG.
- Electrical issues, certain conditions like Wolf Parkinson White Syndrome or implanted pacemakers, can cause inverted T waves due to abnormal electrical pathways in the heart.
- Normal variants Some people naturally have T wave inversions in certain leads of their ECG, and this is not linked to the heart.
- Not all T wave inversions are dangerous, but those accompanied by chest pain, dizziness, or shortness of breath may signal a heart issue that needs urgent attention.
What is the importance of the T wave on an ECG?
T-wave has a special significance in ECG. It represents the ventricular recovery after a contraction. Abnormal T-waves indicate ischemia, electrolyte imbalance, or heart disease
T-waves help to identify heart diseases. They play a vital role in the electrical function and are essential for evaluating heart health because they reflect the recovery phase of the ventricles.
Indicators of heart's electrical health
Flat or inverted T-waves are abnormal electrical impulses in the heart, indicating atrial or ventricular arrhythmias. They warrant urgent medical attention.
- Early detection of ischemia: An inverted T-wave is an early sign of myocardial ischemia. The heart muscles do not get oxygen due to reduced blood flow. Ischemia causes angina or leads to a heart attack.
- Detecting T-wave changes on an ECG requires a quick intervention to prevent heart damage and improve recovery.
- Electrolyte imbalances: Hyperkalemia or hypokalemia (abnormal potassium levels) causes the T-wave to peak or flatten. Calcium imbalance affects the T wave and heart rhythm. Electrolyte imbalances are detected early by observing the T-waves, which prevents complications like arrhythmias or cardiac arrest.
- Assessing cardiac recovery. Normal T-waves indicate proper ventricular recovery, while abnormal prolongation or shape changes indicate heart conditions.
Importance of T wave in clinical settings
T-wave abnormalities indicate early heart conditions, such as
- arrhythmias
- myocardial ischemia
The shape, direction, and amplitude of T-waves help healthcare providers to detect electrolyte imbalances and impaired heart functions. T-wave analysis is important in cardiology as it aids in early intervention and preventive care.
Arrhythmias detection
T-wave abnormalities indicate arrhythmia, where the heart beats irregularly. They point to issues in the heart’s electrical conduction, which causes tachycardia or bradycardia.These deviations help health practitioners decide on medication or pacemakers to prevent complications.
Identifying myocardial ischemia
T-wave analysis helps in the early detection of myocardial ischemia when the heart muscle receives insufficient oxygen due to reduced blood flow. Abnormal T-waves are the first signs of ischemia.
T-wave analysis guides timely interventions like
- Lifestyle changes
- Medications
- Surgical procedures
Dynamic T-wave flattening due to anterior ischemia
T wave flattening reverses as ischemia resolves.
Electrolyte imbalance diagnosis
T-wave changes indicate shifts in electrolyte levels of potassium and calcium. In hyperkalemia, peaked T waves occur, while in hypokalaemia, flattened T waves occur.
GlobalT-wave flattening in hypokalaemia associated with U waves prominent in V2 and V3
Tall peaked Twaves in hyperkalaemia
Monitoring ventricular health
Regular analysis of the T wave helps assess how well the ventricles are recovering after contraction. Any abnormalities in this face indicate ventricular hypertrophy or heart failure. Tracking these changes, clinicians evaluate the progression of heart disease and modify treatment. Improving patient outcomes and helping to prevent further deterioration.
T-wave Abnormalities
They are
- Peaked T-waves
- Hyperacute T-waves
- Inverted T-wave
- Biphasic T-waves.
- Camel hump, T-waves
- Flattened T-waves
Inverted T waves
Inverted T waves are seen in the following conditions.
- Normal finding in children.
- Myocardial ischemia and infarction (including Wellens syndrome.)
- Bundle branch block
- Ventricular hypertrophy.
- Pulmonary embolism
- Hypertrophic cardiomyopathy
- Raised intracranial pressure.
T Wave inversion in the lead III is a normal variant. On comparing with previous ECG, a new T wave inversion is always abnormal. Pathological T wave inversion is symmetrical and deeper than 3 mm
Paediatric T waves
- Inverted T waves in right precordial leads (V1-3) are normal in children
- Represent right ventricle domination of forces
Myocardial ischemia and infarction
They occur in contiguous leads based on the anatomical equation of the area of ischemia.
- Inferior. II, III, aVF
- Lateral I, aVL, V5-6
- Anterior V2-6
The inversions may be
- Dynamic T inversions are seen with acute MI.
- Fixed T wave inversions are seen following infection in association with pathological Q waves.
Inferior T wave inversion due to acute ischemia
Inferior T wave inversion with Q waves-prior MI
T wave inversion in lateral leads due to ischemia
Anterior T wave inversion with Q waves due to recent MI
Bundle Branch Block
Bundle branch block. The heart's electrical signals don't travel normally, causing delays in contraction and changes in how the heart resets (repolarizes). As a result, T-wave inversion, a flipping of the wave that represents recovery, is a normal finding. And does not necessarily indicate heart disease.
It occurs due to appropriate discordance, meaning harmless changes on the ECG, such as T wave inversion and ST segment depression. These changes are typical in bundle branch blocks and do not always suggest a heart attack. However, if certain ECG changes move in the same direction as the heartbeat's electrical activity, it may indicate an underlying heart problem that requires further evaluation.
Left Bundle Branch Block
Causes T wave inversion in lateral leads I, aVL, and V5-6
Right Bundle Branch Block
Causes T wave inversion in the right precordial leads V1- 3
Ventricular Hypertrophy
Left Ventricular Hypertrophy
- Increased LV voltages: huge precordial R and S waves that overlap with the adjacent leads (SV2 + RV6 >> 35 mm).
- R-wave peak time > 50 ms in V5-6 with associated QRS broadening.
- LV strain pattern with ST depression and T-wave inversions in I, aVL, and V5-6.
- ST elevation in V1-3.
- Prominent U waves in V1-3.
- Left axis deviation.
Right Ventricular hypertrophy
- Right axis deviation (+150 degrees).
- Dominant R wave in V1 (> 7 mm tall; R/S ratio > 1)
- Dominant S wave in V6 (> 7 mm deep; R/S ratio < 1).
- Right ventricular strain pattern with ST depression and T-wave inversion in V1-4.
Hypertrophic cardiomyopathy
It is associated with deep T-wave inversions in all precordial leads.
Raised Intracranial Pressure
It produces widespread T-wave inversions with bizarre morphology
Differential Diagnosis of Inverted T-waves in Adults
Inverted T waves on an ECG indicate issues related to myocardial ischemia, left ventricular hypertrophy, or electrolyte imbalances. It necessitates evaluation to determine the exact cause.
Identifying the diagnosis is crucial for intervention and effective management. Proper interpretation of ECG combined with clinical history and additional diagnostic tests is essential to distinguish the specific conditions that may lead to inverted T waves in adult patients.
Myocardial ischemia
When the blood flow to the heart muscle is reduced, myocardial ischemia occurs. It is due to the lack of oxygen to the muscles. Inverted T waves in this condition are common, and patients experience chest pain and discomfort during exertion.
Left ventricular hypertrophy
It is caused by thickening of the left ventricle due to increased workload as a result of hypertension or valvular heart disease. T-wave inversion occurs due to altered electric conduction of the heart. Initially, the patients remained asymptomatic but later developed shortness of breath or chest pain.
Electrolyte imbalances
Hypokalemia or hyperkalemia cause significant changes in cardiac repolarization, leading to inverted T-waves.
- Low potassium levels (hypokalaemia) often result in flattened or inverted T waves.
- Hyperkalemia (high levels of potassium) caused peaked T-waves or vast QRS complexes.
Muscle weakness, fatigue, and palpitations arise because of it. The identification and correction of these imbalances through dietary changes and supplementation restores normal cardiac function and prevents complications.
Pulmonary embolism
It occurs when a blood clot obstructs the pulmonary artery, leading to cardiovascular stress. Precordial leads may show inverted T waves reflecting right ventricular strain. They present with acute shortness of breath, chest pain, or hemoptysis. Treatment includes anticoagulation or thrombolysis to dissolve the clot and restore normal blood flow.
Central nervous system events
The subarachnoid or intracranial hemorrhage causes inverted T waves. They cause considerable stress on the heart's electrical activity, and the patients have headaches, altered consciousness, or focal deficits.
Factors Affecting T Waves
T wave morphology is influenced by the heart’s electrical and physiological state. Changes in T wave shape, amplitude, and direction signal temporary conditions such as electrolyte imbalances or more chronic issues like ischemia.
Electrolyte imbalances
High potassium levels (hyperkalemia) cause peaked T-waves.
Low potassium levels (Hypokalaemia) lead to flat or inverted T-waves
Reduce blood flow
Reduced blood flow to the heart causes injury to cardiac muscles, leading to ischemia.
Age and gender
Women display more pronounced T-waves. As individuals age, the heart's electrical system also changes, altering T wave morphology.
Body position
Lying down versus standing ECG can result in different T wave shapes. It is due to changes in venous return and hard position.
Improper lead placement
It impacts T-wave morphology that does not reflect the heart’s electrical activity.
Preventing T Wave Formation
Preventing T wave inversion is achieved by preventing the disease that leads to its inversion. A healthy diet with balanced meals and adequate exercise are the best ways to prevent a T wave inversion. Other ways to prevent T-wave inversion are to reduce stress and drink plenty of water.
Conclusion
T-wave abnormalities help to detect cardiovascular issues early. The healthcare providers intervene promptly and recognize conditions like ischemia, electrolyte imbalances, and arrhythmias.
Gauze supports the utilization of advanced analytics and real-time monitoring for diagnosis and management of T-wave dysfunction. It integrates data and provides personalized care plans for better patient outcomes
Here to answer all your questions
Primary T-wave inversions are due to electrical changes in the heart. They are caused by ischemia pericarditis, CNS disorders, genetic conditions, or electrolyte imbalances
Yes, T-waves can predict a cardiac event.
T wave abnormalities can be prevented by
- Lifestyle modifications
- Medication adjustments
- Interventions to address underlying conditions.
Gauze.health offers user-friendly tools and insights, empowering patients to track their heart health and make informed lifestyle choices.
It is achieved by a healthy diet with balanced meals and adequate exercise.
Yes, T-waves can predict a cardiac event.
T-wave abnormalities can cause severe conditions like arrhythmias or heart attacks.
Treatments often include lifestyle modifications, medication adjustments, or interventions to address underlying conditions, all facilitated by Gauze.health’s analytics.

